Preparing to have a heart baby at Guys and St Thomas Hospital, London.
The start to 2024, was an intense one as our little family was preparing to welcome our precious, rather complicated, bundle into the world. Little Mathilda had grown beautifully everywhere except in one location – her aorta. The vital location that was responsible for allowing her body to be pumped full of life-giving oxygenated blood was narrow and pinched. So we knew that it was highly likely that she would need surgery soon after birth to reconstruct her aorta.
You know what, the journey of the months after discovering about her needs was a tricky one too… more on that another time. She had coarctation of the aorta and a hypoplastic aortic arch, in case you’re interested.
Three Nights in Neonatal Care Unit
So after birth. Mathilda spent three nights in neonatal NICU… I was in the Post Natal Ward and Duncan was at home in Chiswick juggling Gabriel our three year old with the support of my mum. Mathilda was in a high dependency ward as shortly after birth she had to be cannulated and given prostoglandin, Prostin, which was a hormone to keep a duct open in her heart that bypassed some of the narrowed aorta and helped more oxygenated blood get around.
To be honest, the time in NICU was very difficult. Straight after giving birth we are exhausted, weak, emotional, fragile and anxious about baby being well… let alone to the additional fears and concerns that can come with having a baby with serious medical needs. More on this section another time.

Sky Cardiology Paediatric Ward in Evelina Hospital
It felt like a miracle when I learned that the Paediatric Ward in the adjoining children’s hospital was happy to take Mathilda at three days old. The miracle was that her cubicle included a pull down bed for parents. It was a dream come true. Particularly as I was desperately hoping to establish a positive breastfeeding relationship with Mathilda. Post Natal Ward had been getting ready to kick me out… as their standard policy was 72 hours max unless otherwise needed – I was panicking about being in a completely different building to her and not being able to feed on demand.
She had already proven that all her other organs were functioning well and she was feeding brilliantly too. The only high need issue was the Prostin Line that medically needed to continuous to ensure the duct was open. A Senior Nurse who was also a lactation consultant said that Mathilda was demonstrating organised feeding – with an initial flutter feed followed by regular deeper sucks. This was impressive in a newborn baby. I had been breastfeeding her for two days, after waiting about 24 hours directly after birth. The first 24 hours involved her being syringe fed, with many syringes of colostrum that I had collected before her birth, to manage how much milk she was taking and to avoid overwhelming her gastric digestive system. Anyway, she did beautifully and proved that she had a great digestive system.
So we moved to Sky Ward on Sunday evening.
Positive Choices in Sky Cardiology Paediatric Ward
It was recommended to be up out of bed by about 9:30am – being not even one week post partum, I was pretty tired and sore. However the nurses offered to help put the bed away if I needed help. AND April, the nurse who was Mathilda’s nurse on the night we moved in, got me an extra mattress which I used for the entire stay on my pull out bed. With two mattresses it was pretty comfy.
So my tip here is to GET COMFY.
When we are in such an emotionally uncertain and uncomfortable season in our life, being as physically comfortable as possible is worth it.
- I had about four pillows: two for bedtime, one to sit on and one to prop my arm up when breastfeeding
- My feet and ankles blew up with the elimination of retained water and hormones from pregnancy. As I was sat in a chair beside Mathilda’s bed for most of the day I ended up getting very sore ankles… so we quickly started hunting for a footstool or something to prop up my feet during some windows of the day.
- I had a skinny pregnancy pillow which became my buddy in bed as it was often a bit lonely and having something to cuddle and help comfort me was very useful.
- Make sure you have comfortable shoes and trousers due to all the sitting – we couldn’t carry Mathilda away from her bed well about a metre away was our limit. For three weeks.

Food and Drink
I had a drinks and snack cupboard to help lift my mood, begin and end my day, and season my hospital meals. Breastfeeding mothers could have a hospital meal – three meals a day. Though really it was one parent per patient could have food. This was sometimes a bit sad as I could eat and Duncan couldn’t, even though he was suffering through the journey with me. In my cupboard I had:
- Fruity fizzy water and squash (happy flavours to encourage happy thoughts)
- Cereal and pastries (fun alternative breakfast and tasty evening snacks)
- Biscuits and jelly babies (little boost during the day)
- Marmite and peanut butter (to have with morning toast as the hospital only offers jam and butter or margarine)
- A pot of salt and pepper mix (my sister picked it up when she visited one day… it was great to sprinkle on my hot lunches and dinners)
- Chilli flakes (I use them at home and it was comforting to have them for my meals at hospital, though the pot didn’t have very spicy chilli flakes it was still good)
- A cutlery set (the set you get offered at hospital for meals is either wooden or metal and they don’t feel great, so it is well worth getting a personal set – can be washed in the parents room, or even in the sink in the bathroom).
- Hot chocolate, instant coffee (caffeinated and decaffeinated), Horlicks, earl grey (caffeinated and decaffeinated) and vanilla redbush tea – I start my day with caffeinated coffee, hot chocolate with hot water and milk and usually
- Antiseptic wipes that were given at every hospital meal and I didn’t use it every time
- Left over jam pots from breakfasts at hospital
My Drinking and Eating Routine on the Ward
I’d start my day with caffeinated coffee, hot chocolate with hot water and milk (homemade mocha), and it would be a little mission to get that made before ward round that would happen at about 10-10:30am. Then during the day I’d drink water, squash, fizzy water and caffeinated earl grey. Then into the evening I’d switch to decaf earl grey, red bush tea or decaf mocha. The medical staff became familiar with my regular pilgrimage to the parents kitchen that was down a corridor, through security doors and by the exit of the ward – it was where we could independently get water as there wasn’t a general access water dispenser on the ward, apparently there was no space.
Try, Try, Try to eat three meals a day. Give hospital food a chance if you have the chance.
Slow Down and Enjoy the Simple Moments
In between the observations, heel pricks, feedings, ward rounds, nappy changes and visits from other medical staff, I took the time to stroke her hands and skin. To watch the sun light on her face – thankfully we had full length window, basically a window for a wall. Stroking her helped my mind to slow down and focus on loving her, noticing her sweet newness and dreaming of the peace of home. I would fantasize about laying in our bed in peace… no beeps, strangers and questions… just comfort, adoration and newborn delights.
I would celebrate her cuteness. How content she was. How well she fed. Watching her little hands move and stroke as she fed. When she pulled out her nasal feeding tube after her surgery I was so proud of her. They didn’t put it in again. I felt so proud of her strength. When she would often hold a superman/woman style pose and doctors commented on it, I loved that she was reminding people of her strength.
Advocate for your child’s best interests
There are certain routine observations that are essential, and others that could be argued to be done less. With her heel pricks we realised that some staff were better at doing them than others, so we pushed to have staff do it who were more confident with the task. It mostly helped. Mathilda would struggle so much with it and her cries were awful to bear. She had to have a prostin line through a cannula initially and then they inserted a long line in her right arm which was meant to last about 3 weeks. However in the last few days preceding her surgery, the prostin line began having inclusions which sort of was about kinks in the line stopping smooth transfer of the hormone, or the pressure increased and impacted transfer of the hormone. It was hard and I panicked at first, and then was eventually told that it wasn’t an emergency situation. However the days before her surgery, we allowed staff to try and change her long line into a short term cannula. I sort of regret it as they tried too many times. Even tried to put a line in her skull. It all failed. I was crying in the opposite bed space, attempting to eat dinner. Hangry Elizabeth is dangerous – so I forced myself to eat. We stopped trying with the cannula in the end and she was given new lines all over at the surgery. She had one line on each hand and each foot, she had a big one in her neck and in her inner thigh and she had oxygen, a feeding tube and three drainage tubes. I just flicked through the photos and tears quickly fell with the reminder. I’m proud I got through writing most of this without tears.
Have a chat and switch off
Even though it feels vital to be alert and present at all times for our child, sometimes we need to give ourselves permission to switch off. After the two weeks I felt able to start watching a series on my iPad – it was pleasant to switch off and decompress a little bit. I initially felt guilty, that it was taking me away from tending to Mathilda. However I reminded myself that I was literally sitting next to her and was ready to turn it off and be ready to talk with any medical staff that stopped by.
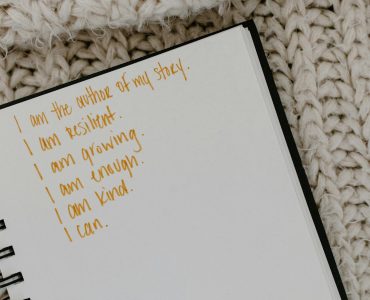
Take a moment to say hello to other parents, lend a listening ear and also to laugh with anyone willing to laugh (if you can), sometimes that was the last thing on my heart/mind and I couldn’t do it. A few times I cleaned the parents kitchen, which was nice as a distraction. Let yourself cry if you need to. Journal if it helps – I couldn’t. It was too painful. I know I’ve missed precious tiny memories by not recording them, but my stomach was clenched and I was too heart broken.
Little note about now
She is well, doing very well now. Next check up is due for the end of the year or early 2025 unless we have concerns. I still feel terribly sad when coming into Waterloo and getting close to the hospital. The corridors have memories in them. The café and shops have tearful moments and are still making them with other families. My heart broke over and over again. I’ll never forget it.